Your Health insurance claim processing system images are ready in this website. Health insurance claim processing system are a topic that is being searched for and liked by netizens today. You can Find and Download the Health insurance claim processing system files here. Get all free photos.
If you’re searching for health insurance claim processing system images information connected with to the health insurance claim processing system interest, you have come to the ideal blog. Our site always provides you with suggestions for seeing the maximum quality video and picture content, please kindly search and locate more informative video content and graphics that fit your interests.
Health Insurance Claim Processing System. At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part. Clearinghouses then scrub, standardize, and screen medical claims before sending them to the payer. Healthcare claims management is a highly complex process. The savings for insurers can be dramatic:
 How About The Benefits Of Using Medical Billing Software From max90hyperfuses.co.uk
How About The Benefits Of Using Medical Billing Software From max90hyperfuses.co.uk
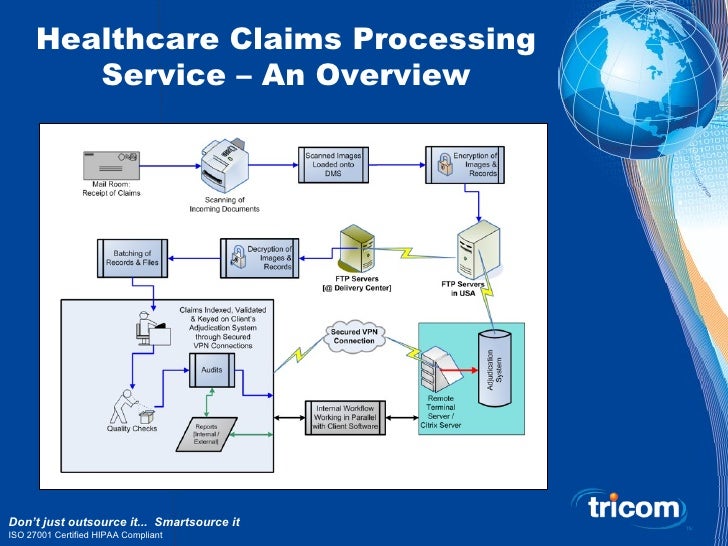
The need for standards in claims processing. Plexis’ claims processing software has the capabilities to achieve your highest business outcomes. Oscar’s claims system was built with the next stage of the healthcare industry in mind. Lemonade claims users can tap a button on the lemonade mobile phone app in order to begin the claims process. In terms of architecture, at least three layers must be configured for health insurance claims processing automation: Features include claims validation, claims adjudication, aggregated data access and handling of denials &.
(assignment 02 onwards) implementing a claim.
The rising cost of claims and the complexity of claims management are among the most pressing challenges health insurance companies and other private payers face today. (assignment 02 onwards) implementing a claim. Lemonade is not a b2b ai vendor, but instead an insurance company themselves. Indian health insurance companies or tpas generally hire medical professionals ranging from pharmacy graduates to alternative systems doctors to mbbs doctors for process claims. At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part. Social security (nhi) regulations 2015;
 Source: coverager.com
Source: coverager.com
Advanced navigation tools the modern healthclaimsxg interface helps operators quickly navigate to the screens they need to process each claim, increasing payment accuracy and reducing costly human errors. At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part. In essence, claims processing refers to the insurance company’s procedure to check the claim requests for adequate information, validation, justification and authenticity. If you’re finding yourself in a. Members’ claims will be processed faster, the healthcare provider will get paid faster, and the insurance company can have fewer pending claims outstanding.
![Information flow of claim data processing [7]. CRS claim Information flow of claim data processing [7]. CRS claim](https://www.researchgate.net/profile/Stuart_Speedie/publication/232746293/figure/download/fig3/AS:202921066143760@1425391560488/Information-flow-of-claim-data-processing-7-CRS-claim-review-support-EDI-electronic.png) Source: researchgate.net
Source: researchgate.net
It will support future product iterations and business lines and enable faster, easier, and more efficient. Clearinghouses then scrub, standardize, and screen medical claims before sending them to the payer. Plexis’ claims processing software has the capabilities to achieve your highest business outcomes. It can be made simple by customized medical claims processing software with the claim integration system. Oscar’s claims system was built with the next stage of the healthcare industry in mind.
 Source: greatoutdoorsabq.com
Source: greatoutdoorsabq.com
Ppos generally have higher premiums, but allow for more flexibility for subscribers. Plexis is a trusted leader in the global healthcare payer community with an average client tenure of over 8 years. Lemonade claims users can tap a button on the lemonade mobile phone app in order to begin the claims process. With its claimscape products, datagenix provides complete claims software for all aspects of health claims processing & benefits management. This stage comprises the journey from a claimant registering a request with the insurance company to the generation of the claim in the insurance company’s database.
 Source: ehealthireland.ie
Source: ehealthireland.ie
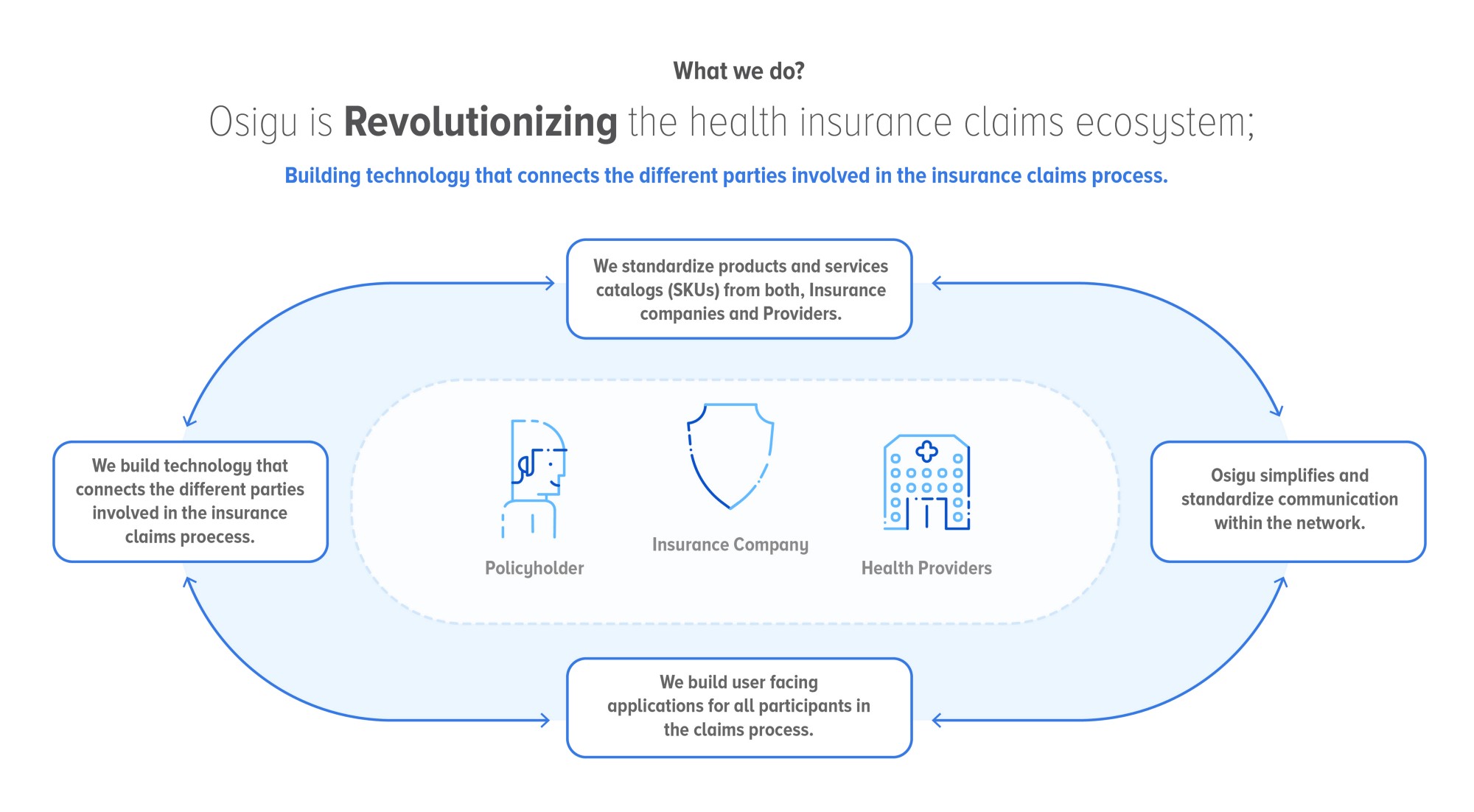
As shown in the above infographic, the entire health insurance claims process can be divided into three stages. In terms of architecture, at least three layers must be configured for health insurance claims processing automation: Our agile claims processing software delivers cost savings through automated enterprise efficiencies. This software is suitable for tpas, asos, ipas & bpos. In essence, claims processing refers to the insurance company’s procedure to check the claim requests for adequate information, validation, justification and authenticity.
 Source: ibmbigdatahub.com
Source: ibmbigdatahub.com
Tailored medical billing systems with claims integration allow easy access to a digital archive of all the records, including medical, dental, prescription, and vision services in the usa. In essence, claims processing refers to the insurance company’s procedure to check the claim requests for adequate information, validation, justification and authenticity. Plexis is a trusted leader in the global healthcare payer community with an average client tenure of over 8 years. When the insurer is first notified, the claims processing life cycle is kicked off. In an increasingly digital world, removing the need to submit paper bills to health insurers offers medical providers and their patients a fantastic opportunity for improvement.
 Source: comindware.com
Source: comindware.com
Ppos recently over took hmos as the most common mco. If you’re finding yourself in a. Insurance claims management software features. Plexis is a trusted leader in the global healthcare payer community with an average client tenure of over 8 years. Digitizing every step of the claims process, from data input to payment, has the potential to streamline claims management, as well as boost its efficiency and accuracy.
 Source: youtube.com
Source: youtube.com
If you’re finding yourself in a. At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part. Features include claims validation, claims adjudication, aggregated data access and handling of denials &. (a) propose a business case of value based care, from a company point of view (assignment 01) (b) your project team has been requested to make the claims processing system icd 10 compliant. Claims software, benefits software and solutions for health benefits payors, tpas, and healthcare insurance companies.
 Source: dontblinkphotoz.blogspot.com
Source: dontblinkphotoz.blogspot.com
Healthcare group has been hired to provide services and built it system healthcare products for a university. Unlike an hmo, subscribers to a ppo may see any doctor, physician or other provider, but they pay less if they see a provider within the ppo’s network (hence “preferred”). (a) propose a business case of value based care, from a company point of view (assignment 01) (b) your project team has been requested to make the claims processing system icd 10 compliant. Numerous client testimonials attest to the unique. Claims software, benefits software and solutions for health benefits payors, tpas, and healthcare insurance companies.
 Source: max90hyperfuses.co.uk
Source: max90hyperfuses.co.uk
Health insurance claim life cycle. Insurance claims is a complicated endeavor requiring great skill and accuracy. These medical professionals use their training and experience to verify a healthcare claim and to determine if the Accurate capture of data and satisfactory user experience are critical. A medical claims clearinghouse is an electronic intermediary between healthcare providers and payers.
 Source: cbinsights.com
Source: cbinsights.com
At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part. The need for standards in claims processing. The savings for insurers can be dramatic: As shown in the above infographic, the entire health insurance claims process can be divided into three stages. Tailored medical billing systems with claims integration allow easy access to a digital archive of all the records, including medical, dental, prescription, and vision services in the usa.
 Source: ehealthireland.ie
They claim they can process claims faster and provide customers with fast payouts using ai, including a chatbot. Digitizing every step of the claims process, from data input to payment, has the potential to streamline claims management, as well as boost its efficiency and accuracy. Numerous client testimonials attest to the unique. Social security (nhi) regulations 2015; Oscar’s claims system was built with the next stage of the healthcare industry in mind.
 Source: hatchingbunniesfarm.blogspot.com
Source: hatchingbunniesfarm.blogspot.com
Plexis’ claims processing software has the capabilities to achieve your highest business outcomes. This software is suitable for tpas, asos, ipas & bpos. Digitizing every step of the claims process, from data input to payment, has the potential to streamline claims management, as well as boost its efficiency and accuracy. The company may also reject the claim request, if found invalid, forged,. With its claimscape products, datagenix provides complete claims software for all aspects of health claims processing & benefits management.
Source: quora.com
Social security (amendment) act 2014; With its claimscape products, datagenix provides complete claims software for all aspects of health claims processing & benefits management. They claim they can process claims faster and provide customers with fast payouts using ai, including a chatbot. In an increasingly digital world, removing the need to submit paper bills to health insurers offers medical providers and their patients a fantastic opportunity for improvement. Social security (nhi) regulations 2015;
Source: visual.ly
In large healthcare systems, one or more employees may be assigned exclusively to handle the processing of health insurance claims. They claim they can process claims faster and provide customers with fast payouts using ai, including a chatbot. Our agile claims processing software delivers cost savings through automated enterprise efficiencies. The need for standards in claims processing. Healthcare providers transmit their medical claims to a clearinghouse.
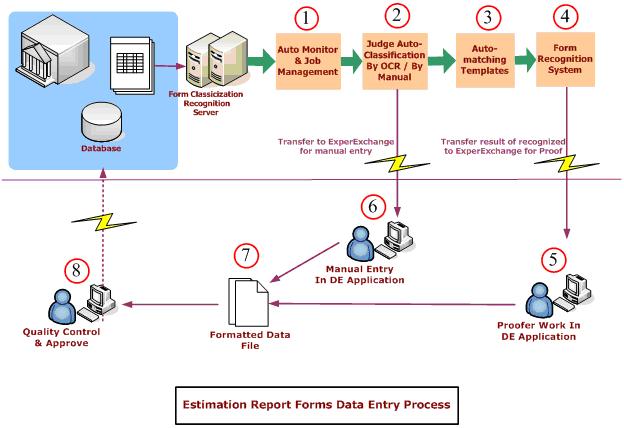 Source: expervision.com
Source: expervision.com
Insurance claims is a complicated endeavor requiring great skill and accuracy. Health insurance claim life cycle. As shown in the above infographic, the entire health insurance claims process can be divided into three stages. Ppos recently over took hmos as the most common mco. Insurance claims management software include the following identifiable features:
 Source: slideserve.com
Source: slideserve.com
If you’re finding yourself in a. Ppos recently over took hmos as the most common mco. This stage comprises the journey from a claimant registering a request with the insurance company to the generation of the claim in the insurance company’s database. Our agile claims processing software delivers cost savings through automated enterprise efficiencies. With its claimscape products, datagenix provides complete claims software for all aspects of health claims processing & benefits management.
 Source: slideshare.net
Source: slideshare.net
In essence, claims processing refers to the insurance company’s procedure to check the claim requests for adequate information, validation, justification and authenticity. The need for standards in claims processing. If you’re finding yourself in a. Social security (amendment) act 2014; Healthcare group has been hired to provide services and built it system healthcare products for a university.
 Source: blog.bcbsnc.com
Source: blog.bcbsnc.com
The need for standards in claims processing. They claim they can process claims faster and provide customers with fast payouts using ai, including a chatbot. A large portion of the population maintains healthcare insurance in order to be protected from major financial loss from medical bills. Healthcare group has been hired to provide services and built it system healthcare products for a university. The need for standards in claims processing.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site value, please support us by sharing this posts to your own social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title health insurance claim processing system by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.