Your Experimental treatments not covered by insurance images are ready. Experimental treatments not covered by insurance are a topic that is being searched for and liked by netizens today. You can Find and Download the Experimental treatments not covered by insurance files here. Find and Download all free images.
If you’re searching for experimental treatments not covered by insurance pictures information connected with to the experimental treatments not covered by insurance interest, you have pay a visit to the ideal blog. Our website always provides you with hints for seeking the maximum quality video and picture content, please kindly search and find more informative video content and images that match your interests.
Experimental Treatments Not Covered By Insurance. Experimental treatments are not covered by many policies, even when those treatments have proven to be the best or only solution to a medical problem. Most health plans don’t cover treatments they regard as “experimental.” sometimes, they may deny a claim for such a treatment. When employers provide insurance coverage, the employee often does not automatically receive a copy of the health plan, within which there are usually exclusions of coverage. Moreover, insurers may try to claim that a treatment is experimental even when it has been accepted by mainstream medical society.
 ANTHOXANTHUM ODORATUM COVER POSTTREATMENT AT EXPERIMENTAL From researchgate.net
ANTHOXANTHUM ODORATUM COVER POSTTREATMENT AT EXPERIMENTAL From researchgate.net
Most health plans don’t cover treatments they regard as “experimental.” sometimes, they may deny a claim for such a treatment. If you’ve been told your treatment isn’t covered because it’s investigational or experimental, you may still have recourse. Emergency use ind authorizes use of an experimental drug when time is not sufficient for the usual application process. Ask the insurance company what other treatments they are most frequently denying as experimental. If you join an approved trial, most health plans can’t limit your benefits or. If your insurer says your therapy is experimental, you can appeal and try to get it covered.
Medicare typically does not cover experimental and investigational procedures.
The issue has come to light as a number of people have been recommended experimental treatment, only to find that the insurer will not cover it. Emergency use ind authorizes use of an experimental drug when time is not sufficient for the usual application process. Medicare typically does not cover experimental and investigational procedures. As a general rule, experimental treatments are not. I shouldn’t be paying for these treatments out of pocket.” Bcbsnc does not cover investigational (experimental) services.
 Source: military.net
Source: military.net
The family’s subsequent lawsuit against the insurance company has been unsuccessful. Get a free 2022 open enrollment guide written by christian simmons Because these treatments and medications cannot be established as effective for a large group of patients, the cost of covering them is not justifiable. Private health insurance plans vary quite a bit. If your insurer says your therapy is experimental, you can appeal and try to get it covered.
Source: escolabressolelrial.blogspot.com
Most health plans don’t cover treatments they regard as “experimental.” sometimes, they may deny a claim for such a treatment. Many insurers deny legitimate claims for coverage based on a treatment being “experimental,” but the real reason is because they don’t want to incur high costs of coverage. Experimental treatments involve “sliding scale” considerations. The family’s subsequent lawsuit against the insurance company has been unsuccessful. Here are steps for getting your insurer to pay for your treatment.
 Source: cartoonstock.com
Source: cartoonstock.com
If you join an approved trial, most health plans can’t limit your benefits or. The issue has come to light as a number of people have been recommended experimental treatment, only to find that the insurer will not cover it. Read the provisions in your insurance contract. Here are steps for getting your insurer to pay for your treatment. Moreover, insurers may try to claim that a treatment is experimental even when it has been accepted by mainstream medical society.
 Source: ritterim.com
Source: ritterim.com
The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. “insurance companies should not be able to turn down experimental surgeries and treatments,” she said. Insurers typically have an appeals process. The family’s subsequent lawsuit against the insurance company has been unsuccessful. You and your provider may be able to show proof that the therapy works.
 Source: nottinghamoncology.co.uk
Source: nottinghamoncology.co.uk
The family’s subsequent lawsuit against the insurance company has been unsuccessful. Emergency use ind authorizes use of an experimental drug when time is not sufficient for the usual application process. When employers provide insurance coverage, the employee often does not automatically receive a copy of the health plan, within which there are usually exclusions of coverage. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Medicare typically does not cover experimental and investigational procedures.
 Source: researchgate.net
Source: researchgate.net
Experimental treatments involve “sliding scale” considerations. Read the provisions in your insurance contract. Medicare also covers some of the costs associated with participating in clinical trials. Experimental treatments are not covered by many policies, even when those treatments have proven to be the best or only solution to a medical problem. Insurers typically have an appeals process.
 Source: adrenogate.net
Source: adrenogate.net
Then, you have grounds for an appeal. Then, you have grounds for an appeal. The most important thing to understand when treatment is denied is that an insurer’s initial denial of coverage because a treatment is “experimental” is not the final word on the subject. Ask the insurance company what other treatments they are most frequently denying as experimental. Experimental and investigational procedures, items and medications are not covered.
 Source: researchgate.net
Source: researchgate.net
Insurers typically have an appeals process. A service is considered investigational (experimental) if any of the following criteria are met: The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. If your insurer says your therapy is experimental, you can appeal and try to get it covered. Many health insurers decline coverage for experimental medical treatments simply because there is not enough evidence of success to warrant deeming them medically necessary.
 Source: careplus.att.com
Source: careplus.att.com
Insurance coverage for experimental treatments. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Emergency use ind authorizes use of an experimental drug when time is not sufficient for the usual application process. Experimental treatments involve “sliding scale” considerations. Health plan contracts typically have exclusions for treatments that an insurance company considers “investigational” or “experimental.” health plans say there is insufficient proof demonstrating that certain treatments are safe and effective for their intended use, making them investigational or experimental and not a covered medical benefit.
 Source: slideshare.net
Source: slideshare.net
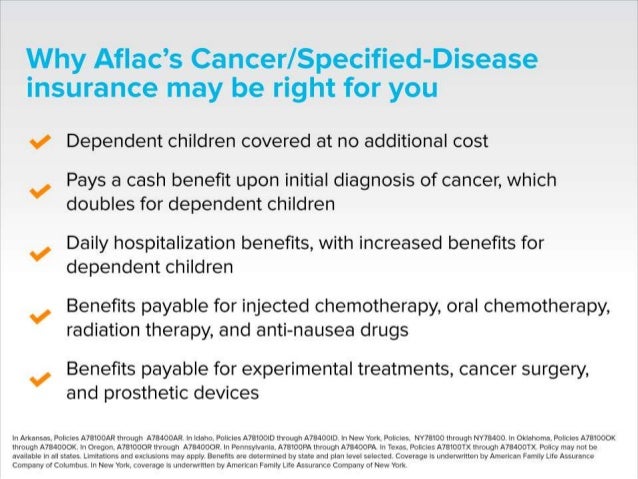
The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. For coverage of drugs and biologicals, refer to the coverage summaries titled. Insurance coverage for experimental treatments. Get a free 2022 open enrollment guide written by christian simmons Medications/drugs (outpatient/part b) and chemotherapy, and associated drugs and treatments.
 Source: cancertodaymag.org
But, you and your doctor may think the treatment is well supported by evidence. Traditionally, private medical insurance companies would not cover what they deemed to be experimental treatments but it looks that will be changing, as this article explains. Insurers typically have an appeals process. But, you and your doctor may think the treatment is well supported by evidence. Most health plans don’t cover treatments they regard as “experimental.” sometimes, they may deny a claim for such a treatment.
 Source: academia.edu
Source: academia.edu
Because these treatments and medications cannot be established as effective for a large group of patients, the cost of covering them is not justifiable. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Medicare typically does not cover experimental and investigational procedures. Many health insurers decline coverage for experimental medical treatments simply because there is not enough evidence of success to warrant deeming them medically necessary. When employers provide insurance coverage, the employee often does not automatically receive a copy of the health plan, within which there are usually exclusions of coverage.
 Source: expresspharma.in
Source: expresspharma.in
Many health insurers decline coverage for experimental medical treatments simply because there is not enough evidence of success to warrant deeming them medically necessary. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. A service is considered investigational (experimental) if any of the following criteria are met: Insurance coverage for experimental treatments. Then, you have grounds for an appeal.
 Source: slideshare.net
Source: slideshare.net
Many insurers deny legitimate claims for coverage based on a treatment being “experimental,” but the real reason is because they don’t want to incur high costs of coverage. For coverage of drugs and biologicals, refer to the coverage summaries titled. The most important thing to understand when treatment is denied is that an insurer’s initial denial of coverage because a treatment is “experimental” is not the final word on the subject. Private health insurance plans vary quite a bit. Experimental and investigational procedures, items and medications are not covered.
 Source: wpln.org
Source: wpln.org
As a general rule, experimental treatments are not. Because these treatments and medications cannot be established as effective for a large group of patients, the cost of covering them is not justifiable. Medicare also covers some of the costs associated with participating in clinical trials. I shouldn’t be paying for these treatments out of pocket.” Experimental and investigational procedures, items and medications are not covered.
 Source: dailymail.co.uk
Source: dailymail.co.uk
Investigational device exemption (ide) studies category a device Here are steps for getting your insurer to pay for your treatment. The issue has come to light as a number of people have been recommended experimental treatment, only to find that the insurer will not cover it. The family’s subsequent lawsuit against the insurance company has been unsuccessful. Health plan contracts typically have exclusions for treatments that an insurance company considers “investigational” or “experimental.” health plans say there is insufficient proof demonstrating that certain treatments are safe and effective for their intended use, making them investigational or experimental and not a covered medical benefit.
 Source: hiltonheadcosmeticdentistry.com
Source: hiltonheadcosmeticdentistry.com
Such therapies are usually looked at as nontraditional or experimental. Most health plans don’t cover treatments they regard as “experimental.” sometimes, they may deny a claim for such a treatment. Such therapies are usually looked at as nontraditional or experimental. Insurance coverage for experimental treatments. You and your provider may be able to show proof that the therapy works.
 Source: researchgate.net
Source: researchgate.net
Moreover, insurers may try to claim that a treatment is experimental even when it has been accepted by mainstream medical society. Insurance coverage for experimental treatments. Investigational device exemption (ide) studies category a device Medicare also covers some of the costs associated with participating in clinical trials. Insurers typically have an appeals process.
This site is an open community for users to submit their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site beneficial, please support us by sharing this posts to your own social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title experimental treatments not covered by insurance by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.