Your Does insurance cover ablation images are ready in this website. Does insurance cover ablation are a topic that is being searched for and liked by netizens today. You can Get the Does insurance cover ablation files here. Download all royalty-free images.
If you’re searching for does insurance cover ablation images information related to the does insurance cover ablation keyword, you have visit the ideal site. Our website frequently provides you with hints for seeking the maximum quality video and image content, please kindly hunt and find more informative video articles and graphics that fit your interests.
Does Insurance Cover Ablation. Most insurers will cover a hysterectomy as long as it’s medically necessary and your doctor recommends it. Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding. Also question is, is vein ablation covered by insurance? The answer is yes, varicose vein treatment is covered by most commercial insurance carriers such as blue cross blue shield, champus, aetna, cigna, humana, health net, tricare, umr, and unitedhealthcare to name a few.
 The ClosureFast ™ procedure to treat leg veins is also From pinterest.com
The ClosureFast ™ procedure to treat leg veins is also From pinterest.com
Ligation with or without stripping. This scarring reduces or prevents bleeding. Endometrial ablation should not be done in women who are past menopause and is not recommended for those with the following medical conditions: Endometrial ablation with or without hysteroscopic guidance is considered medically necessary if the medical appropriateness criteria are met. The typical procedure for removing varicose veins is ablation (radiofrequency ablation or endovenous laser ablation). If you don’t have insurance or if your insurance won’ (3).
Insurance companies have different requirements to grant an authorization, but they typically require that your specialist documents the following:
Medicare coverage for radiofrequency ablation. Whether or not your insurance company will cover these newest procedures is yet to be determined. In a couple of years, these new vein procedures will obtain their own insurance codes to be eligible for insurance coverage. As with any medical procedure, we always recommended calling your insurance company to have them explain your coverage. (see medical appropriateness below.) endometrial ablation with or without hysteroscopic guidance for the treatment of other conditions/diseases is considered. It should also be noted that these are general criteria and each insurance policy can be different.
 Source: palisadesveincenter.com
Source: palisadesveincenter.com
Yes, adenomyosis causes significant pain and extremely heavy bleeding. Endometrial ablation should not be done in women who are past menopause and is not recommended for those with the following medical conditions: Medicare recipients may need to show that other treatments have. It can also be used for other types of bleeding in the uterus. Ligation with or without stripping.
 Source: veindirectory.org
Source: veindirectory.org
Medicare recipients may need to show that other treatments have. If you have had a surgical ablation, insurance companies want to know if there are any other issues such as heart disease. The vast majority of these posts are quite positive, and the names of certain practitioners come up again and again. Treatment of spider veins (telangiectases) sclerotherapy for cosmetic purposes. It can also be used for other types of bleeding in the uterus.
 Source: morning-news-215.blogspot.com
Source: morning-news-215.blogspot.com
A maximum of five (5) facet joint injection sessions inclusive of medial branch blocks, intraarticular injections, facet cyst rupture and rf ablations may be performed per year in the cervical/thoracic spine and five (5) in the lumbar spine. This scarring reduces or prevents bleeding. Medicare recipients may get coverage for radiofrequency ablation if the procedure is deemed medically necessary by your physician. Most insurers will cover a hysterectomy as long as it’s medically necessary and your doctor recommends it. Similarly, can anyone get an endometrial ablation?
 Source: vaveinandvascular.com
Source: vaveinandvascular.com
Does insurance cover endometrial ablation? Insurance companies have different requirements to grant an authorization, but they typically require that your specialist documents the following: As it heals, the lining will scar. Does insurance cover endometrial ablation? It should also be noted that these are general criteria and each insurance policy can be different.
 Source: morning-news-215.blogspot.com
Source: morning-news-215.blogspot.com
Also question is, is vein ablation covered by insurance? As podiatrists, we do not perform these venous ablation procedures but we often refer venous ulceration patients to vein clinics and/or vascular surgeons. (see medical appropriateness below.) endometrial ablation with or without hysteroscopic guidance for the treatment of other conditions/diseases is considered. Similarly, can anyone get an endometrial ablation? Ablation works by destroying the lining of your uterus.
 Source: pinterest.com
Source: pinterest.com
Medicare coverage for radiofrequency ablation. If after the ultrasound, your physician determined that an endovenous ablation is needed then those procedures have higher costs and thus it would likely be in your best interest to bill those to insurance and have them applied to your deductible. If you have had a surgical ablation, insurance companies want to know if there are any other issues such as heart disease. Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding. The answer is yes, varicose vein treatment is covered by most commercial insurance carriers such as blue cross blue shield, champus, aetna, cigna, humana, health net, tricare, umr, and unitedhealthcare to name a few.
 Source: austinvaricosevein.com
Source: austinvaricosevein.com
Medicare will cover these treatments for varicose veins when deemed medically necessary: As with any medical procedure, we always recommended calling your insurance company to have them explain your coverage. The answer is yes, varicose vein treatment is covered by most commercial insurance carriers such as blue cross blue shield, champus, aetna, cigna, humana, health net, tricare, umr, and unitedhealthcare to name a few. For example, the following criteria may need to be met before rfa is approved for coverage when using the technique for pain. Medicare coverage for radiofrequency ablation.
 Source: bassmedicalgroup.com
Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding. Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding. In these cases, after documentation of venous insufficiency by ultrasound, medicare will usually deem endovenous ablation and ambulatory phlebectomy to be medically necessary. Medicare coverage for radiofrequency ablation. Whether or not your insurance company will cover these newest procedures is yet to be determined.
 Source: thesecretveinclinic.com
Source: thesecretveinclinic.com
We will post any coverage updates from private insurance companies on our website, so check back frequently. Recommendations for insurance coverage of varicose vein treatments that involve radiofrequency ablation, endovenous laser treatment and microphlebectomies. Part of your first visit to vein clinics of america is for us to review your insurance benefits with you. Most insurers now cover endovenous thermal ablation treatment as a primary treatment and sclerotherapy as a secondary treatment, when deemed medically necessary. Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding.
 Source: georgiamtc.com
Source: georgiamtc.com
We will post any coverage updates from private insurance companies on our website, so check back frequently. For insurance to cover these procedures, they usually require an authorization. If after the ultrasound, your physician determined that an endovenous ablation is needed then those procedures have higher costs and thus it would likely be in your best interest to bill those to insurance and have them applied to your deductible. If you have had a surgical ablation, insurance companies want to know if there are any other issues such as heart disease. It�s not recommended if you plan to get pregnant.
 Source: vipmedicalgroup.com
Source: vipmedicalgroup.com
It can also be used for other types of bleeding in the uterus. It can also be used for other types of bleeding in the uterus. Whether or not your insurance company will cover these newest procedures is yet to be determined. Part of your first visit to vein clinics of america is for us to review your insurance benefits with you. Endometrial ablation with or without hysteroscopic guidance is considered medically necessary if the medical appropriateness criteria are met.
 Source: regionvein.com
Source: regionvein.com
As it heals, the lining will scar. A maximum of five (5) facet joint injection sessions inclusive of medial branch blocks, intraarticular injections, facet cyst rupture and rf ablations may be performed per year in the cervical/thoracic spine and five (5) in the lumbar spine. Does insurance cover endometrial ablation? Yes, adenomyosis causes significant pain and extremely heavy bleeding. If you have had a surgical ablation, insurance companies want to know if there are any other issues such as heart disease.
 Source: southwestveinandleg.com
Source: southwestveinandleg.com
It can also be used for other types of bleeding in the uterus. The answer is yes, varicose vein treatment is covered by most commercial insurance carriers such as blue cross blue shield, champus, aetna, cigna, humana, health net, tricare, umr, and unitedhealthcare to name a few. Medicare will cover these treatments for varicose veins when deemed medically necessary: Endometrial ablation should not be done in women who are past menopause and is not recommended for those with the following medical conditions: If you have had a surgical ablation, insurance companies want to know if there are any other issues such as heart disease.
 Source: veinscarolina.com
Source: veinscarolina.com
Endometrial ablation is a type of procedure that�s often used to treat heavy menstrual bleeding. It�s not recommended if you plan to get pregnant. Is endometrial ablation covered by insurance? (see medical appropriateness below.) endometrial ablation with or without hysteroscopic guidance for the treatment of other conditions/diseases is considered. Most insurers now cover endovenous thermal ablation treatment as a primary treatment and sclerotherapy as a secondary treatment, when deemed medically necessary.
 Source: saviderm.com
Source: saviderm.com
The vein institute of new jersey is considered one of the top vein. Criteria for approval varies depending on the condition rfa is being used to treat. Part of your first visit to vein clinics of america is for us to review your insurance benefits with you. This scarring reduces or prevents bleeding. Yes, adenomyosis causes significant pain and extremely heavy bleeding.
 Source: cbsnews.com
Source: cbsnews.com
For example, the following criteria may need to be met before rfa is approved for coverage when using the technique for pain. I need some help please! Medicare will cover these treatments for varicose veins when deemed medically necessary: Medicare coverage for radiofrequency ablation. For example, the following criteria may need to be met before rfa is approved for coverage when using the technique for pain.
 Source: metroveincenters.com
Source: metroveincenters.com
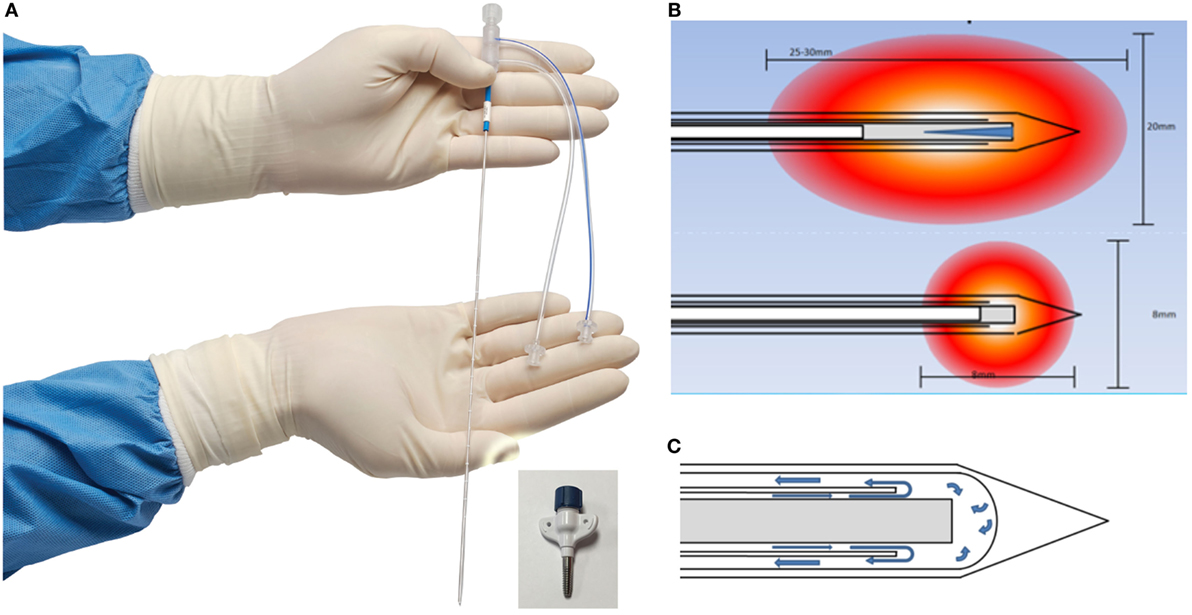
(see medical appropriateness below.) endometrial ablation with or without hysteroscopic guidance for the treatment of other conditions/diseases is considered. Special ablation tools are then inserted and used to treat atrial fibrillation triggers. If you don’t have insurance or if your insurance won’ (3). Medicare recipients may need to show that other treatments have. The vast majority of these posts are quite positive, and the names of certain practitioners come up again and again.
 Source: austinvaricosevein.com
Source: austinvaricosevein.com
Also question is, is vein ablation covered by insurance? If after the ultrasound, your physician determined that an endovenous ablation is needed then those procedures have higher costs and thus it would likely be in your best interest to bill those to insurance and have them applied to your deductible. As a result, insurance should cover the costs of vein ablation. For example, medicare does not cover: In a couple of years, these new vein procedures will obtain their own insurance codes to be eligible for insurance coverage.
This site is an open community for users to submit their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site good, please support us by sharing this posts to your preference social media accounts like Facebook, Instagram and so on or you can also save this blog page with the title does insurance cover ablation by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.