Your Do insurance companies pay for experimental treatments images are ready. Do insurance companies pay for experimental treatments are a topic that is being searched for and liked by netizens now. You can Find and Download the Do insurance companies pay for experimental treatments files here. Find and Download all royalty-free photos.
If you’re looking for do insurance companies pay for experimental treatments pictures information connected with to the do insurance companies pay for experimental treatments keyword, you have visit the ideal site. Our site always gives you hints for downloading the highest quality video and picture content, please kindly surf and find more enlightening video articles and images that fit your interests.
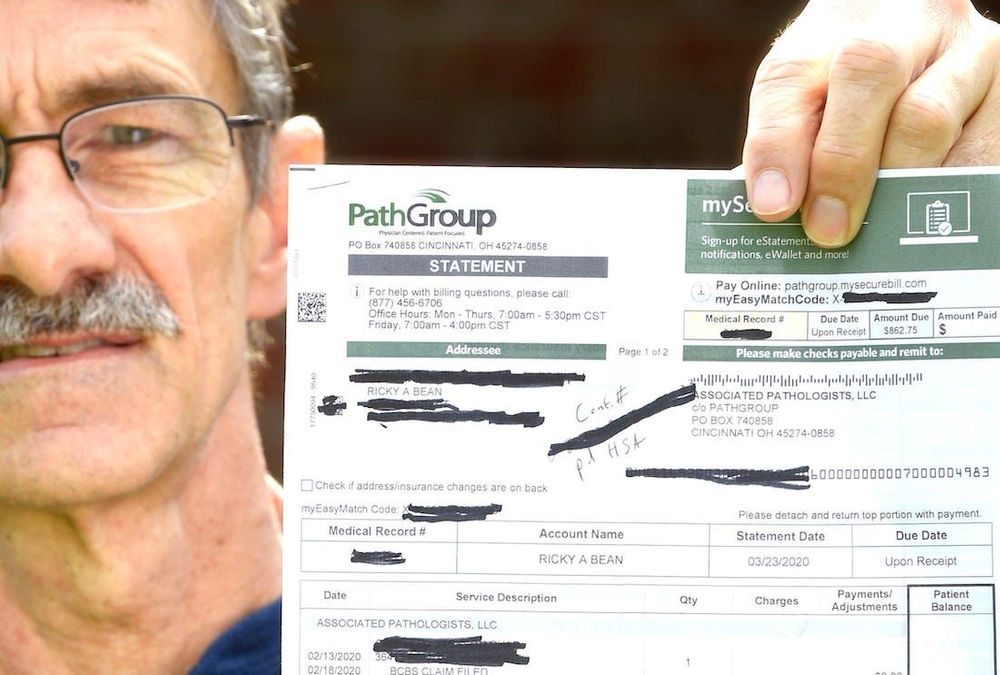
Do Insurance Companies Pay For Experimental Treatments. Here are steps for getting your insurer to pay for your treatment. The trial must be an approved clinical trial. The unproven definition, however, excludes treatments: It�s not unusual — insurers often require that a medical procedure be thoroughly tested and proven effective before they decide to cover it.
 Does Insurance Cover Saliva Hormone Testing How to Guide From rotarianseclubfellowship.org
Does Insurance Cover Saliva Hormone Testing How to Guide From rotarianseclubfellowship.org
Ask the insurance company what other treatments they are most frequently denying as experimental. You must be eligible for the trial. The fast answer to the question is that insurance limits our ability to help patients. Insurers won’t pay for experimental treatment. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. A second final rule prohibits drug manufacturers from asking patients to pay a profit or for research and development costs.
It’s important to understand what an experimental or investigational treatment is so you can prepare a convincing appeal if you were to be denied treatment.
The family’s subsequent lawsuit against the insurance company has been unsuccessful. Insureds is seen in the dispute over experimental treatments. That’s a gap in your prescription drug coverage. In actuality, there may be abundant evidence showing the treatment is beneficial, including case studies in the medical literature, clinical research, and anecdotal evidence from doctors. But, often, the trial sponsor will supply the investigational treatment free of charge. Experimental treatments and health insurance coverage.
 Source: f.apecwln.org
Source: f.apecwln.org
As a result, insurance companies may end up taking a blanket approach when denying claims for experimental treatment (without considering the needs of their patients). United healthcare insurance company uses an exclusion in its medical policies for treatments it considers “experimental or investigational or unproven.” the investigational definition merely requires that the treatment have approval from an appropriate regulatory body such as the fda. Insurers argue that if they paid for experimental treatment, they would be subsidizing medical research and paying for unproven treatments. From our obsession “america first” by annalisa merelli senior reporter published may 30, 2018this article is more than 2 years old. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract.
 Source: revisi.net
Read the provisions in your insurance contract. Experimental treatments and health insurance coverage. As a result, insurance companies may end up taking a blanket approach when denying claims for experimental treatment (without considering the needs of their patients). Many health insurers decline coverage for experimental medical treatments simply because there is not enough evidence of success to warrant deeming them medically necessary. It’s important to understand what an experimental or investigational treatment is so you can prepare a convincing appeal if you were to be denied treatment.
 Source: thebalancecareers.com
Source: thebalancecareers.com
Experimental treatments and health insurance coverage. But, often, the trial sponsor will supply the investigational treatment free of charge. The family’s subsequent lawsuit against the insurance company has been unsuccessful. An orphan drug is an already approved or experimental drug for treatment of conditions affecting less than 200,000 people in the country. “insurance companies should not be able to turn down experimental surgeries and treatments,” she said.
 Source: notyouraveragenutritionist.com
Source: notyouraveragenutritionist.com
Insurers won’t pay for experimental treatment. Because these treatments and medications cannot be established as effective for a large group of patients, the cost of covering them is not justifiable. 4 thoughts on “ if you die from coronavirus ‘vaccine’, your life insurance won’t pay as it’s an ‘experimental medical intervention’ ” mark schumacher in. It�s not unusual — insurers often require that a medical procedure be thoroughly tested and proven effective before they decide to cover it. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract.
 Source: liputan6.nanyamulu.com
Source: liputan6.nanyamulu.com
4 thoughts on “ if you die from coronavirus ‘vaccine’, your life insurance won’t pay as it’s an ‘experimental medical intervention’ ” mark schumacher in. Ask the insurer to explain what is experimental about this procedure. The trial must be an approved clinical trial. But, often, the trial sponsor will supply the investigational treatment free of charge. Many health insurers decline coverage for experimental medical treatments simply because there is not enough evidence of success to warrant deeming them medically necessary.
 Source: buzzgoat.com
Source: buzzgoat.com
Usually, you’ll keep on getting routine care from your own. In other situations, treatments must be proven effective before a health insurance company will pay for them. The family’s subsequent lawsuit against the insurance company has been unsuccessful. It’s important to understand what an experimental or investigational treatment is so you can prepare a convincing appeal if you were to be denied treatment. Insurers won’t pay for experimental treatment.
 Source: rotarianseclubfellowship.org
Source: rotarianseclubfellowship.org
It�s a question patients ask us all the time: Unfortunately, insurers often end up taking a blanket approach when it comes to certain types of treatments, denying entire areas of treatment even where there is evidentiary support for effectiveness in certain situations. There is a special status for a drug intended to treat rare diseases. The unproven definition, however, excludes treatments: Insurers won’t pay for experimental treatment.
 Source: pinterest.com
Source: pinterest.com
The family’s subsequent lawsuit against the insurance company has been unsuccessful. In other situations, treatments must be proven effective before a health insurance company will pay for them. United healthcare insurance company uses an exclusion in its medical policies for treatments it considers “experimental or investigational or unproven.” the investigational definition merely requires that the treatment have approval from an appropriate regulatory body such as the fda. Because these treatments and medications cannot be established as effective for a large group of patients, the cost of covering them is not justifiable. Experimental treatments and health insurance coverage.
 Source: grantsformedical.com
Source: grantsformedical.com
Experimental treatments and health insurance coverage. A favorite excuse of insurance carriers is that the treatment is “experimental,” and there is not enough evidence showing that the treatment is safe and effective. But, often, the trial sponsor will supply the investigational treatment free of charge. That’s a gap in your prescription drug coverage. The unproven definition, however, excludes treatments:
 Source: harrisandross.co.uk
Source: harrisandross.co.uk
Insurers won’t pay for experimental treatment. From our obsession “america first” by annalisa merelli senior reporter published may 30, 2018this article is more than 2 years old. The fast answer to the question is that insurance limits our ability to help patients. Insurers won’t pay for experimental treatment. Federal law requires most health insurance plans to cover routine patient care costs in clinical trials under certain conditions.
 Source: youtube.com
Source: youtube.com
The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Insurers won’t pay for experimental treatment. It’s important to understand what an experimental or investigational treatment is so you can prepare a convincing appeal if you were to be denied treatment. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. An orphan drug is an already approved or experimental drug for treatment of conditions affecting less than 200,000 people in the country.
 Source: doctorwhoblog.com
Source: doctorwhoblog.com
The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Ask the insurer to explain what is experimental about this procedure. Insurance companies will not pay for experimental drugs. Ask the insurance company what other treatments they are most frequently denying as experimental. There is a special status for a drug intended to treat rare diseases.
 Source: f.apecwln.org
Source: f.apecwln.org
The employer, if involved, desires to have the appearance The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. Insurers won’t pay for experimental treatment. But, often, the trial sponsor will supply the investigational treatment free of charge. As a result, insurance companies may end up taking a blanket approach when denying claims for experimental treatment (without considering the needs of their patients).
 Source: e.apecwln.org
Source: e.apecwln.org
Ask the insurance company what other treatments they are most frequently denying as experimental. Experimental treatments and health insurance coverage. But, often, the trial sponsor will supply the investigational treatment free of charge. The trial must be an approved clinical trial. Ask the insurer to explain what is experimental about this procedure.
 Source: c.lebanonpartnership.org
Source: c.lebanonpartnership.org
Insurance companies will not pay for experimental drugs. Why doesn�t insurance cover natural medicine? Usually, you’ll keep on getting routine care from your own doctor, and your insurer should continue to pay for that. I shouldn’t be paying for these treatments out of pocket.” You must be eligible for the trial.
 Source: robinsonandhenry.com
Source: robinsonandhenry.com
Here are steps for getting your insurer to pay for your treatment. Another major concern cancer patients face is the maximum benefit provided by the insurance company. Federal law requires most health insurance plans to cover routine patient care costs in clinical trials under certain conditions. Usually, you’ll keep on getting routine care from your own. From our obsession “america first” by annalisa merelli senior reporter published may 30, 2018this article is more than 2 years old.
 Source: rotarianseclubfellowship.org
Source: rotarianseclubfellowship.org
The trial must be an approved clinical trial. Experimental treatments and health insurance coverage. The insurance company justified the refusal of payment to the family by stating that the use of experimental medication or treatments, including corona injections, is expressly excluded from the insurance contract. The fast answer to the question is that insurance limits our ability to help patients. The trial must be an approved clinical trial.
 Source: revisi.net
Source: revisi.net
That’s a gap in your prescription drug coverage. Another major concern cancer patients face is the maximum benefit provided by the insurance company. As a result, insurance companies may end up taking a blanket approach when denying claims for experimental treatment (without considering the needs of their patients). Insurers won’t pay for experimental treatment. From our obsession “america first” by annalisa merelli senior reporter published may 30, 2018this article is more than 2 years old.
This site is an open community for users to do submittion their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site helpful, please support us by sharing this posts to your preference social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title do insurance companies pay for experimental treatments by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.